LA County Department of Public Health (DPH) Director Barbara Ferrer held a COVID-19 briefing on Thursday afternoon, Jan. 20, touching on a wide range of topics about the ongoing pandemic.
Here are seven key things Ferrer said during the video conference:
“I’m really hopeful that we’re plateauing.”
Ferrer said that, although testing delays from the Martin Luther King Jr. Holiday weekend meant DPH still did not have complete data, some signs seemed to point toward a plateau after a skyrocketing COVID-19 case rate that has been recorded in LA County since mid December.
“Around January 8, January 9, is when we had our highest daily case rates, when we go back and figure out at what point did someone either test or have symptoms,” Ferrer said. “That would be encouraging for us, because that would mean that we really are in a plateau right now. I’d love to see signs that we’re in a real decline, but I think we have to wait to get a complete week’s worth of data here.”
By the numbers: as of Thursday, the average daily new case rate was about 33,000 cases a day; test positivity decreased slightly over the past week to 17 percent; the seven-day average daily case rate fell slightly to 350 new cases per 100,000 residents.
An additional 102 COVID-19 related deaths were reported on Thursday in LA County. Most of those are thought to have been infected with the omicron variant of the virus.
“We’re still experiencing the highest rate of spread for this entire pandemic.”
Ferrer said that the omicron variant began spreading among travelers, event attendees and people out socializing, but is now primarily spreading among people who work or live in close proximity to others.
“At the beginning of December and early on in the spread of omicron, while we still had a fair amount of Delta circulating, those most likely to become infected often were travelers, those attending entertainment venues and those intermingling in places where many were close together while unmasked,” Ferrer said. “Some of the recent shifts associated with widespread community transmission likely reflect the fact that we’re now seeing increased transmission among those whose jobs are putting them in close contact with others and who often live in crowded housing.” Ferrer said those areas included South and Central LA, East LA and parts of the Valley.
“There are likely to be more outbreaks in the weeks to come at our schools.”
LA County was tracking 24 active school outbreaks countywide as of Thursday, but Ferrer said high rates of community spread meant more school outbreaks — where three or more cases were linked to a known exposure at a school or a school-sanctioned event — were likely before the omicron surge subsided.
Ferrer stressed the importance of vaccines throughout her remarks on Thursday.
“To ensure safety at our schools, I want to note that there are over 140 school-based vaccine clinics that are scheduled just this week, and we have nearly 500 school-based vaccine clinics scheduled for the month of February,” Ferrer said.
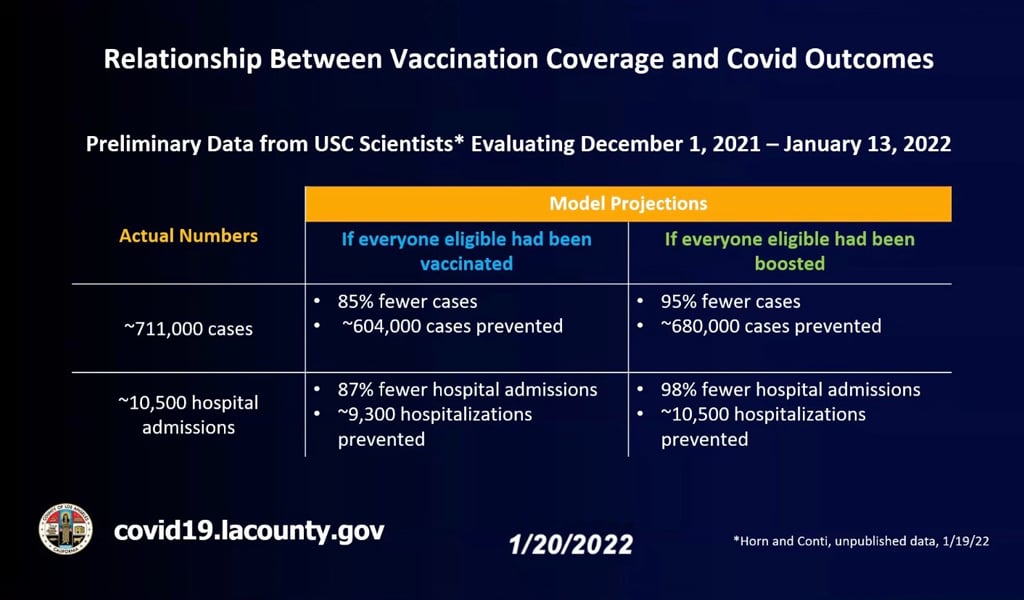
“When looking at cases, estimates from the model predict that if everyone eligible were vaccinated, there would have been 85 percent fewer cases, or approximately 604,000 cases of COVID-19, prevented between Dec. 1 and Jan. 13.”
USC scientists provided DPH with a model that showed the impact vaccinations have had on the spread of the virus; the preliminary data (which Ferrer said was complex and not precise) showed that full vaccine compliance could have had a dramatic impact on the rates of COVID-19 in LA County over the past six weeks.
Full vaccinations for all eligible Angelenos would have resulted in 87 percent fewer hospitalizations in that time period, according to the model; when it came to boosters, the model predicted there would have been 96 percent fewer cases and 98 percent fewer hospitalizations had every eligible Angeleno received a booster shot.
Ferrer said the data was able to “show just how much impact large scale vaccine adoption at a population level could have on the pandemic’s trajectory, our case and hospitalization reductions, and ultimately, can help lead to the end of the pandemic.”
“If you have members of your family who are at very high risk, this would be the time to probably do a delay, unless you can get everyone tested right before you gather.”
With the Lunar New Year coming up on Feb. 1, a reporter for the LA Times asked Ferrer if DPH had updated guidance for the annual holiday, which usually sees thousands of LA-area families gathering with family members.
Ferrer said moving celebrations outdoors was safer than gathering indoors, and again reinforced the role of vaccinations in avoiding high rates of spread, but said the department did not have specific guidelines directing residents to not attend such gatherings.
“For some people, this time is just very risky — and that includes people who are unvaccinated, particularly if they’re older, particularly if they have underlying health conditions, or they’re immunocompromised,” Ferrer said.
“There’s also new opportunities for residents to now receive in-home antigen test kits.”
LA County residents were encouraged to visit covid19.la.gov/testing. There, an at-home test can be ordered or residents can locate nearby testing centers.
A set of four at-home tests per valid address are available through the Federal government by visiting covidtests.gov.
Ferrer also noted insurance companies are now required to reimburse customers for up to eight rapid tests per month, at up to $12 per test (with slightly different rules for companies that use a network of pharmacies).
“We’re seeing a much shorter time frame, and that’s tragic. It means that for the people who are in fact ending up passing away from COVID, if they were infected with omicron, it looks like they get hit pretty hard earlier on.”
According to Ferrer, for those who have died after being infected with the omicron variant, the length of time between exposure and death is shorter than for those who have died after being infected with earlier versions of the virus, including the delta variant.
She estimated that about 80 of the 102 people whose COVID-19-related deaths were reported on Thursday had been infected after Jan. 1, meaning they had been sick for 19 days or fewer before dying from the disease.
Because the death rate is considered a lagging indicator, Ferrer said the fact that deaths were rising faster than had been expected may mean the death rate could also fall faster than had been expected — but only time could tell.
emily@smdp.com